Introduction:
Rovadicitinib (TQ05105) is a first-in-class, oral, small molecule JAK/ROCK inhibitor which inhibits cell proliferation, induces cell apoptosis and decreases inflammatory cytokines by affecting the JAK-STAT signaling pathway in preclinical studies. Here we report the primary results of the phase I/Ib study of rovadicitinib in Myeloproliferative Neoplasms (MPN) patients.
Methods:
We conducted a single arm, multicenter, open-label, phase I/Ib trial (NCT04339400) at 9 sites in China. The study included dose-escalation cohort (phase I) and dose-expansion cohort (phase Ib). Aged ≥18 with MPN, dynamic international prognostic scoring system (DIPSS) Int-1 or higher risk of MF, naïve or resistant/intolerant to hydroxyurea and/or interferon therapy of PV or ET, were enrolled. Patients with MF must have palpable splenomegaly (≥5 cm below the left costal margin). Eligible patients received escalating doses of oral rovadicitinib 5 mg QD, 5 mg BID,10 mg BID, 15 mg BID, 20 mg BID of each 28-day cycle, and a modified “3 + 3” design was used in phase I. Treatment continued until progressive disease or unacceptable toxicity. The primary outcomes were the maximum tolerated dose (MTD) and recommended phase 2 dose (RP2D) in phase I, and the proportion of patients whose reduction of at least 35% in spleen volume (SVR35) at week 24 compared with baseline in phase Ib. The main secondary end point was proportion of patients whose Total Symptom Score decreased ≥ 50% (TSS50) at week 24 in phase Ib.
Results:
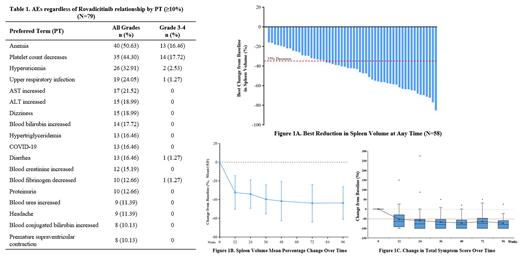
Between November 20, 2018, and September 22, 2022, 102 patients were assessed for eligibility across two cohorts, 79 were enrolled and treated with rovadicitinib including, 15 patients in t phase I and 64 in phase Ib. 50 (63%) patients were male. The median age was 59 years (IQR 50-65), and 16 (20%) patients were aged 65 years or older. All patients had a definite diagnosis during the screening period, 64 (81%) patients were MF (55 were PMF, five were post-PV MF, four were post-ET MF), 10 (13%) patients were ET, five (6%) patients were PV. Mutations of JAK2, CALR, and MPL were analyzed, 60 (76%) of 79 patients with JAK2 V617F mutations, 10 (13%) patients with CALR mutations, four (5%) patients with MPL mutations. The median spleen volume was 1907 cm 3 (IQR 964-2994). In phase I, the number of patients enrolled per dose level was one at 5 mg QD, three at 5 mg BID, four at 10 mg BID, three at 15 mg BID, and four at 20 mg BID. The dose-limiting toxicities (DLTs) were experienced by two patients at 20 mg BID (one patient experienced grade 3 platelet count decrease with bleeding, one patient experienced grade 4 platelet count decrease). Given the safety profile and shrinking spleen, 15 mg BID was identified as MTD and RP2D. Rovadicitinib plasma peak concentrations and areas under the concentration versus time curve increased proportionally with dose. Terminal half-life was 1.3 h. No accumulation trend was noted. In phase Ib, 58 patients were included spleen volume set, 56 patients were included TSS set. 63.79% (37/58) patients achieved SVR35 during the study period (Figure 1A). The proportion of patients who had SVR35 was 37.93% (22/58) at week 24 and 39.66% (23/58) at week 48, respectively. The mean duration of splenic response was approximately 16 months. 87.5% (49/56) patients achieved TSS50 during the study period. The proportion of patients who had TSS50 was 71.43% (40/56) at week 24 and 48.21% (27/56) at week 48, respectively. Patients had durable splenic responses and significant symptom responses. The most common treatment-emergent adverse events (TEAEs) were 1~2 grade (Table 1). Grade ≥3 TEAEs were reported in 39 (49%) patients, the most common grade ≥3 hematological TEAE (≥10%) were platelet count decrease (17.72%) and anemia (16.46%). Occurrence of other grade ≥3 non-hematologic TEAEs was very low. There was only one death, due to disease progression and not related to rovadicitinib. TEAEs were generally manageable.
Conclusions:
Rovadicitinib was generally safe, well-tolerated and showed meaningful clinical activity in patients with MF, especially with palpable splenomegaly. Rovadicitinib may be a new treatment option for myelofibrosis patients. Furthermore, a randomized double-blind phase 2 study is ongoing, aiming to assess the efficacy and safety of rovadicitinib compared to hydroxyurea in patients with intermediate-2 or high-risk myelofibrosis in China (NCT05020652).
Disclosures
Wang:Chia Tai Tianqing Pharmaceutical Group Co., Ltd: Current Employment. Ding:Chia Tai Tianqing Pharmaceutical Group Co., Ltd: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal